Clinical documentation is the cornerstone of healthcare, ensuring accurate patient records, legal accountability, and effective communication among care teams. It guides treatment decisions, supports billing, and enhances patient safety, making it essential for delivering high-quality care.
1.1 Importance of Clinical Documentation in Healthcare
Clinical documentation is fundamental to healthcare, ensuring accurate, complete, and timely records. It supports patient care decisions, legal accountability, and communication among providers. Proper documentation enhances patient safety, reduces errors, and facilitates continuity of care. It also serves as a legal record, protecting both patients and providers. Additionally, it aids in billing, compliance, and quality improvement initiatives, making it indispensable for effective healthcare delivery and operational efficiency.

1.2 Overview of Clinical Documentation Standards
Clinical documentation standards ensure consistency, accuracy, and compliance with legal and regulatory requirements. These standards emphasize the importance of detailed patient histories, accurate diagnoses, and clear treatment plans. They also cover essential elements like progress notes, medication records, and consent forms. Compliance with guidelines from organizations like AHDI and AHIMA is crucial. Standards promote the use of precise terminology, such as ICD-10 codes, and adherence to CMS documentation guidelines, ensuring high-quality patient care and legal accountability. Proper documentation practices are vital for maintaining patient trust and operational efficiency in healthcare settings.
Best Practices for Clinical Documentation
Accurate, complete, and timely documentation is essential for guiding treatment decisions, ensuring patient safety, and maintaining legal compliance. It enhances communication among healthcare teams and protects both patients and providers.
2.1 Principles of Accurate and Complete Documentation
Accurate documentation ensures that patient records reflect the true nature of care provided, while completeness guarantees all relevant details are included. Timeliness, legibility, and objectivity are equally crucial. Documentation should be clear, concise, and free from bias, capturing the patient’s history, diagnosis, treatment plans, and progress. These principles support continuity of care, legal compliance, and accurate billing. They also protect healthcare providers by providing a defensible record of their actions and decisions, ensuring transparency and accountability in patient management.
2.2 Tips for Effective Clinical Documentation
Effective clinical documentation begins with clear, concise, and organized writing. Use templates and automation tools to streamline the process. Focus on capturing essential details like patient history, diagnoses, and treatment plans. Prioritize accuracy and specificity to avoid ambiguity. Regularly review and update records to reflect ongoing care. Use standardized terminology and ensure compliance with regulatory guidelines. Maintain objectivity by documenting facts rather than assumptions. Finally, proofread to eliminate errors and ensure legibility. These practices enhance communication, improve patient outcomes, and support legal and financial requirements.
2.3 Avoiding Common Errors in Documentation
Common documentation errors include inaccuracies, omissions, and lack of clarity. To avoid these, ensure all entries are factual, complete, and free from ambiguity. Use precise language and avoid vague terms. Regularly review records for consistency and accuracy. Address gaps in documentation promptly and verify information with reliable sources. Utilize templates and checklists to guide the process. Proofread entries to catch errors before finalizing. By adopting these practices, healthcare professionals can enhance the reliability and integrity of clinical documentation, improving patient care and compliance with standards.
Essential Clinical Documentation Elements
Clinical documentation must include patient history, assessment, diagnosis, treatment plans, progress notes, and compliance with guidelines, ensuring comprehensive and accurate records for quality care and legal standards.
3.1 Patient History and Assessment
Patient history and assessment are foundational elements of clinical documentation, requiring thoroughness and accuracy. They include the chief complaint, history of present illness, review of systems, past medical history, medications, allergies, and vital signs. Accurate documentation ensures continuity of care, informs diagnosis, and supports treatment planning. It also facilitates legal compliance and effective communication among healthcare providers. Detailed and organized patient histories help clinicians make informed decisions, ensuring high-quality care and patient safety. Proper assessment documentation is critical for tracking progress and meeting regulatory standards.
3.2 Diagnosis and Treatment Plans
Accurate and clear documentation of diagnoses and treatment plans is crucial for guiding patient care and ensuring continuity. It must include specific diagnoses, rationale for treatments, and expected outcomes. Detailed plans should outline medications, therapies, and follow-up steps, aligning with clinical guidelines and patient needs. Proper documentation supports legal compliance, facilitates communication among providers, and ensures alignment with coding systems like ICD-10-CM for accurate reimbursement. Clear documentation also helps track patient progress and adapts to changing conditions, enhancing overall care quality and patient safety.
3.4 Progress Notes and Ongoing Care Documentation
Progress notes and ongoing care documentation are essential for tracking patient progress, adjusting treatment plans, and ensuring continuity of care. These entries should be concise, accurate, and timely, reflecting changes in the patient’s condition, responses to interventions, and any modifications to the care plan. Proper documentation supports effective communication among healthcare providers, enhances patient safety, and ensures legal compliance. It also serves as a reference for future care decisions, making it a critical component of comprehensive clinical documentation practices.
Clinical Documentation Improvement (CDI) Programs
Clinical Documentation Improvement (CDI) programs enhance the accuracy and completeness of patient records, ensuring alignment with coding guidelines and improving reimbursement processes in healthcare organizations.
4.1 What is CDI and Its Role in Healthcare?
Clinical Documentation Improvement (CDI) programs are initiatives aimed at enhancing the accuracy, completeness, and consistency of patient records. CDI ensures that clinical documentation aligns with coding guidelines, improving reimbursement processes and compliance. By focusing on precise and detailed documentation, CDI programs help healthcare organizations achieve accurate patient data, which is critical for quality care, billing, and regulatory compliance. Effective CDI also supports better patient outcomes by ensuring that medical decisions are based on comprehensive and reliable information.
4.2 Benefits of Implementing CDI Programs
Implementing Clinical Documentation Improvement (CDI) programs offers numerous benefits, including enhanced financial performance, reduced compliance risks, and improved patient care quality. CDI ensures accurate and comprehensive documentation, leading to correct coding and reimbursement. It also minimizes gaps in clinical information, supporting better decision-making and patient outcomes. Additionally, CDI programs strengthen revenue cycle management by aligning documentation with billing processes, reducing claim denials, and optimizing resource utilization. Overall, CDI fosters a more efficient and transparent healthcare system, benefiting both providers and patients.
4.3 Key Steps for Successful CDI Implementation
Successful CDI implementation requires a structured approach. First, establish clear goals and engage stakeholders, including clinicians and coders. Provide comprehensive training on documentation standards and coding guidelines. Conduct regular audits to identify gaps and improve accuracy. Implement feedback mechanisms to address documentation deficiencies promptly. Utilize technology, such as EHR templates, to streamline processes. Monitor progress and adjust strategies to ensure sustainability. Continuous improvement and collaboration are essential for maximizing the impact of CDI programs on patient care and financial outcomes.

The Role of Healthcare Professionals in Documentation
Healthcare professionals are crucial in maintaining accurate and comprehensive records, ensuring accountability, and facilitating clear communication. Their documentation directly impacts patient care quality and legal compliance.
5.1 Responsibilities of Clinicians in Maintaining Records
Clinicians are responsible for ensuring accurate, complete, and timely documentation of patient care. This includes recording medical histories, diagnoses, treatments, and outcomes. Proper documentation guides treatment decisions, communicates patient information across care teams, and ensures legal and regulatory compliance. Clinicians must adhere to established guidelines and standards, maintaining patient confidentiality and data integrity. Accurate records also support billing, quality improvement, and continuity of care. Clinicians should regularly review and update documentation, ensuring it reflects the patient’s current condition and care plan; This accountability is vital for delivering safe, high-quality healthcare.
5.2 Engaging Physicians in the Documentation Process
Engaging physicians in clinical documentation is crucial for accuracy and completeness. Physicians should actively participate in documenting patient encounters, ensuring that medical decisions and treatments are clearly recorded. Their involvement enhances the quality of care and supports compliance with regulatory standards. Training physicians on documentation best practices and reducing administrative burdens can improve their engagement. Encouraging collaboration between physicians and other healthcare professionals fosters a culture of transparency and accountability, ultimately benefiting patient outcomes and streamlining workflows.
5.3 Nursing and Allied Health Professionals’ Contributions
Nursing and allied health professionals play a vital role in clinical documentation by providing detailed, accurate, and timely records of patient care. Their documentation includes vital signs, treatments, and patient responses, ensuring continuity of care. These professionals bring a unique perspective, capturing nuanced observations that inform treatment decisions. Their contributions enhance communication among healthcare teams, support compliance with regulations, and improve patient outcomes. By maintaining thorough and precise records, they are essential to the integrity and effectiveness of clinical documentation.

Legal and Compliance Aspects of Clinical Documentation
Clinical documentation must comply with legal standards, ensuring patient privacy and accurate records. Non-compliance can lead to legal consequences, making adherence to regulations crucial for healthcare providers.
6.1 Legal Implications of Inaccurate Documentation
Inaccurate clinical documentation can lead to legal consequences, including fines and lawsuits. It may result in patient harm, miscommunication, and non-compliance with regulations. Providers face liability for negligence or fraud if records are incomplete or misleading. Inaccurate documentation can also compromise patient trust and lead to legal action. Ensuring precise and thorough records is critical to avoid legal repercussions and maintain patient safety. Compliance with legal standards is essential to prevent such risks and uphold the integrity of healthcare services.

6.2 Compliance with Regulatory Guidelines
Compliance with regulatory guidelines is crucial for clinical documentation to ensure adherence to legal and industry standards. Accurate and complete records must align with CMS documentation guidelines, ICD-10 codes, and federal regulations. Non-compliance can result in penalties, audits, and reimbursement issues. Proper documentation ensures that services are appropriately billed and that patient care meets required standards. Regulatory bodies emphasize the importance of precise records to maintain integrity in healthcare delivery and billing processes. Adhering to these guidelines protects both healthcare providers and facilities from legal and financial risks.
6.3 Protecting Patient Privacy in Documentation
Protecting patient privacy in clinical documentation is essential to maintain trust and comply with regulations like HIPAA and GDPR. Sensitive information must be securely stored and accessed only by authorized personnel. Documentation should avoid unnecessary details about patients’ personal lives unless relevant to care. Redacting or encrypting sensitive data ensures confidentiality. Training healthcare staff on privacy practices is critical to prevent breaches. Adhering to these measures safeguards patient confidentiality and upholds legal standards, fostering a secure environment for healthcare delivery and record-keeping.

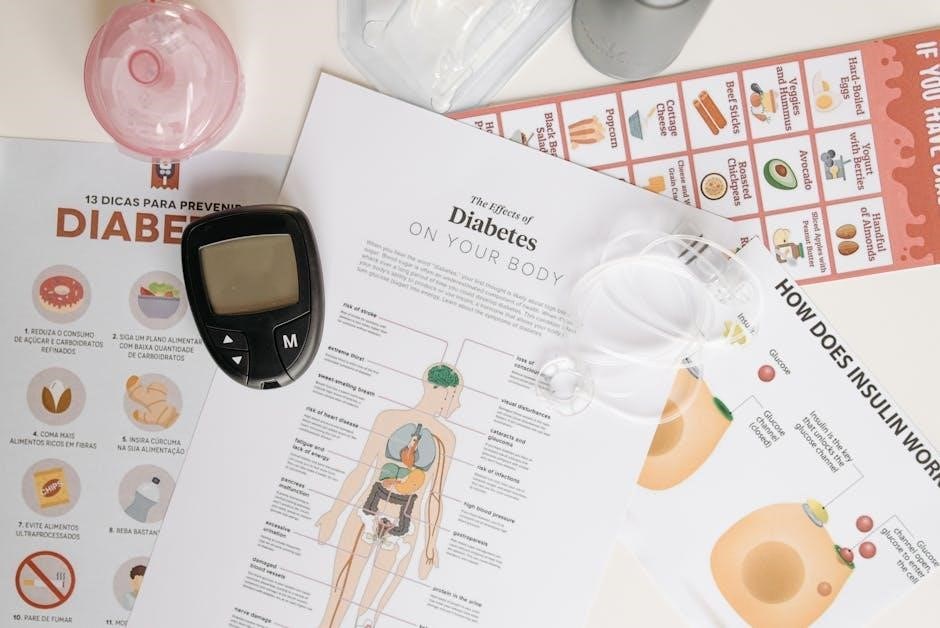
Technological Advancements in Clinical Documentation
Electronic Health Records (EHRs) and automation tools have revolutionized clinical documentation, enhancing accuracy, efficiency, and accessibility. These technologies streamline workflows, reduce errors, and support better patient care outcomes.
7.1 Electronic Health Records (EHRs) and Their Impact
EHRs have transformed clinical documentation by enabling secure, real-time access to patient data, improving accuracy, and streamlining workflows. They reduce administrative burdens, enhance communication, and support informed decision-making. EHRs also facilitate compliance with regulatory requirements and promote continuity of care. By integrating templates and automation tools, they minimize documentation errors and save time, allowing healthcare providers to focus on patient care. Overall, EHRs are pivotal in modernizing healthcare, ensuring efficient and high-quality documentation practices.
7.2 Using Templates and Automation Tools
Templates and automation tools streamline clinical documentation, reducing errors and saving time. Standardized templates ensure consistency, while automation fills in repetitive data, enhancing efficiency. These tools support compliance with regulatory guidelines and improve the accuracy of diagnoses and treatment plans. By minimizing manual entry, they allow clinicians to focus on patient care. Automation also aligns with CDI programs, ensuring precise coding and billing. These innovations are crucial for maintaining high-quality, efficient, and compliant documentation practices in modern healthcare settings.
7.3 The Future of Clinical Documentation Technology
The future of clinical documentation technology lies in advanced tools like AI, machine learning, and natural language processing. These innovations will automate data entry, improve accuracy, and enhance decision-making. AI-driven systems can analyze free-text notes, reducing errors and ensuring compliance. Clinicians will benefit from real-time insights and reduced administrative burdens. As these technologies evolve, they will streamline workflows, improve patient care, and set new standards for documentation efficiency, shaping the next generation of healthcare delivery.
Financial Implications of Clinical Documentation
Accurate clinical documentation is crucial for proper billing, reimbursement, and reducing financial risks. It ensures compliance with regulations and supports efficient revenue cycle management in healthcare settings.
8.1 Impact on Billing and Reimbursement
Accurate clinical documentation directly influences billing and reimbursement processes. Precise coding, such as ICD-10 and CPT, relies on detailed records to ensure proper claims submission. Incomplete or inaccurate documentation can lead to denied claims, delayed payments, or reduced revenue. Compliance with CMS guidelines is essential to avoid financial penalties. Proper documentation alignment with medical necessity ensures correct reimbursement, safeguarding healthcare organizations’ financial stability and operational efficiency. This underscores the critical role of clinical documentation in maintaining fiscal integrity and adherence to regulatory standards.
8.2 Reducing Financial Risks Through Proper Documentation
Proper clinical documentation significantly reduces financial risks by minimizing denied claims, audits, and legal penalties. Accurate records ensure compliance with regulatory guidelines, preventing costly disputes. Detailed documentation supports medical necessity, reducing reimbursement denials. It also mitigates risks associated with incomplete or ambiguous records, which can lead to financial losses. By ensuring clarity and precision, proper documentation safeguards healthcare organizations from economic vulnerabilities, promoting financial stability and operational efficiency.
8.3 The Role of Documentation in Revenue Cycle Management
Clinical documentation plays a pivotal role in revenue cycle management by ensuring accurate billing and reimbursement. Proper documentation aligns ICD-10 codes, CPT/HCPCS, and medical necessity, supporting compliance with CMS guidelines. Detailed records reduce denied claims and audits, streamlining the billing process. Accurate documentation also enhances transparency, ensuring healthcare organizations receive appropriate reimbursement for services provided. By maintaining precise and comprehensive records, documentation directly contributes to financial stability and operational efficiency in the revenue cycle management process.
Patient Care Outcomes and Documentation
Accurate and complete documentation enhances patient care quality by guiding treatment decisions, ensuring safety, and facilitating clear communication among healthcare teams, ultimately improving overall patient outcomes and satisfaction.
9.1 How Documentation Affects Patient Care Quality
Accurate and thorough clinical documentation is critical for delivering high-quality patient care. It ensures that healthcare providers have access to complete and reliable information, enabling informed treatment decisions. Clear records help prevent errors, improve patient safety, and facilitate continuity of care. Effective documentation also supports legal and compliance requirements, protecting both patients and providers. By maintaining detailed and precise records, healthcare teams can enhance communication, reduce misunderstandings, and ultimately improve patient outcomes and satisfaction. Quality documentation is essential for achieving optimal care and operational efficiency in healthcare settings.
9.2 Improving Patient Safety Through Accurate Records
Accurate clinical documentation is vital for ensuring patient safety. Clear and precise records help prevent errors, such as medication mix-ups or misdiagnoses, by providing a reliable source of patient information. Complete documentation ensures continuity of care, reducing gaps that could lead to harm. It also facilitates effective communication among healthcare teams, minimizing misunderstandings. By maintaining accurate records, healthcare providers can identify potential risks early, implement safety measures, and improve overall patient outcomes. Reliable documentation is a cornerstone of safe, high-quality care.
9.3 Enhancing Communication Among Healthcare Teams
Accurate and complete clinical documentation serves as a central communication hub for healthcare teams. It ensures that all providers involved in a patient’s care have access to the same information, promoting consistency and reducing misunderstandings. Clear records facilitate seamless handoffs, consultations, and collaborative decision-making. By documenting patient histories, treatment plans, and progress, clinicians create a shared understanding of patient needs. This enhances teamwork, reduces errors, and ensures that care is coordinated effectively. Effective documentation strengthens communication, ultimately improving patient outcomes and care quality.
Ethical Considerations in Clinical Documentation
Clinical documentation requires transparency, honesty, and respect for patient confidentiality. Ethical practices ensure accurate, unbiased records, fostering trust and accountability while safeguarding sensitive information.
10.1 Maintaining Patient Trust Through Transparent Documentation
Transparent documentation is the foundation of patient trust, ensuring honesty and accountability in care. Clear, accurate, and accessible records allow patients to understand their treatment and feel confident in their providers. By openly sharing information, healthcare professionals demonstrate respect for patient autonomy and confidentiality. Transparent documentation also fosters collaboration between patients and clinicians, promoting shared decision-making. Trust is further strengthened when documentation reflects patient preferences and values, creating a partnership rooted in openness and mutual respect. This ethical approach enhances patient satisfaction and overall care quality.
10.2 Ethical Dilemmas in Documenting Sensitive Information
Documenting sensitive patient information often presents ethical dilemmas, balancing confidentiality with the need for transparency. Clinicians must navigate issues like disclosing mental health diagnoses or substance abuse details, which could impact patient privacy or stigma. There’s also the challenge of maintaining patient autonomy while ensuring accurate records. Breaching confidentiality can erode trust, while withholding information may compromise care quality. Clear ethical guidelines and policies are essential to guide clinicians in making decisions that respect patient rights while upholding legal and professional standards.
10.3 The Clinician’s Moral Responsibility in Recording Care
Clinicians bear a moral responsibility to ensure documentation is truthful, accurate, and respectful. This duty extends beyond legal obligations, encompassing the ethical imperative to represent patients’ stories faithfully. Honest documentation fosters trust, promotes continuity of care, and safeguards patient rights. It also protects clinicians from potential legal or professional repercussions. By adhering to ethical standards, clinicians uphold the integrity of healthcare records, ensuring that care is both patient-centered and accountable. This commitment to moral responsibility is fundamental to maintaining the highest standards of medical practice and patient trust.
Case Studies and Real-World Examples
Real-world examples highlight the impact of accurate documentation, showcasing how it improves patient outcomes, reduces errors, and enhances financial reimbursement in healthcare settings effectively;
11.1 Successful Implementation of CDI Programs
Successful CDI programs ensure accurate and comprehensive documentation, enhancing patient care and financial outcomes. By engaging clinicians and leveraging technology, these programs improve documentation quality, reduce errors, and align with coding standards like ICD-10-CM. Regular training, feedback, and monitoring are key to sustained success, ensuring compliance and optimal reimbursement. Effective CDI programs also foster collaboration between healthcare teams, promoting a culture of precision and transparency in patient records.
11.2 Lessons Learned from Documentation Errors
Documentation errors can lead to legal, safety, and financial repercussions, emphasizing the need for accuracy and completeness. Incomplete records may result in dangerous patient outcomes, while inaccurate data can lead to billing issues and compliance violations. Tools like the “Documentation Matters Toolkit” highlight the importance of proper documentation practices. These lessons underscore the necessity of ongoing training, clear guidelines, and regular audits to prevent errors and maintain high standards of patient care and operational integrity.
11.3 Best Practices in Action: Real-World Scenarios
Real-world scenarios demonstrate how best practices in clinical documentation improve patient care and operational efficiency. For instance, using templates like the Clinical Documentation Cheat Sheet ensures consistency and accuracy. Automation tools, such as those mentioned in the Documentation Matters Toolkit, streamline workflows, reducing errors. Guides like the Clinical Documentation Sourcebook provide sample forms for every stage of treatment, from intake to discharge. These tools and strategies highlight the practical application of effective documentation, fostering better communication and compliance in healthcare settings.
Clinical documentation remains vital for healthcare quality and compliance. As standards evolve, embracing technology like EHRs and automation will shape future practices, ensuring accurate, efficient, and patient-centered care.
12.1 The Evolving Landscape of Clinical Documentation
Clinical documentation is advancing rapidly, driven by technological innovations and regulatory demands. The shift from manual to digital systems, like EHRs, enhances accuracy and accessibility. Automation tools and AI streamline processes, reducing errors and improving efficiency. As standards evolve, documentation must adapt to ensure compliance and patient safety. Staying updated with emerging technologies and best practices is crucial for healthcare professionals to maintain high-quality, patient-centered care in a dynamic environment.
12.2 The Importance of Continuous Improvement
Continuous improvement in clinical documentation is vital for maintaining accuracy, compliance, and patient care quality. Regular updates to documentation practices ensure alignment with changing regulations and technological advancements. By identifying gaps and implementing feedback, healthcare providers can enhance documentation standards. Ongoing training and education empower staff to adapt to new guidelines, reducing errors and improving efficiency. This proactive approach fosters a culture of excellence, ensuring that documentation remains a reliable foundation for patient care and operational success.
12.3 Final Thoughts on Mastering Clinical Documentation
Mastering clinical documentation requires a commitment to accuracy, compliance, and patient-centered care. By leveraging tools like EHRs and CDI programs, healthcare professionals can enhance documentation quality. Continuous learning and adaptation to evolving standards are essential. Ethical considerations, such as transparency and patient privacy, must remain at the forefront. Ultimately, effective documentation is not just a regulatory requirement but a cornerstone of quality care, ensuring clear communication and better patient outcomes. Ongoing improvement and a focus on innovation will shape the future of clinical documentation.

Be First to Comment